Abstract

Detectable MRD during chemotherapy is considered to be the most important prognostic factor in ALL. Pts with molecular failure (MolF) have a poorer overall survival (OS), inferior remission duration (RD) and poorer prognosis even after stem cell transplantation (SCT) compared to pts with molecular CR (MolCR) (Gökbuget et al, Blood 2012: 120(9): 1868). Little is known however on the outcome of pts with MRD results not fitting in the above categories e.g. MRD low positive and on the impact of additional treatments in pts with MolF.
We report an expanded cohort of pts treated according to protocol 07/03 (within the trial or in GMALL registry). MRD was tested by real-time PCR of clonal TCR and Ig gene rearrangements in a reference laboratory (Kiel). The analysis refers to molecular response in 'wk 16' after induction/1st consolidation and to molecular relapse (MolR) later than wk 16 (all definitions see table). The GMALL recommended referral of MolF and MolR pts to SCT in CR1.
The median age of 2061 pts with Ph-neg ALL (1484 trial, N=577 registry) was 34 (16-65) yrs. Pts < 18 yrs (3%) were included until 2012 only. 90% (N=1857) achieved a CR, early death and failure rates were 5% respectively (resp). OS and RD were 60% and 64% at 5 yrs resp. 57% of the CR pts (N=1057) had an MRD test in wk 16. The rate of MRD tests increased over the yrs (2003-2009: 53% vs 2010-2016:69%; p<.0001) as prognostic relevance became more evident.
625 (59%)/1857 pts had a MolCR and196 (18%) MolF. In addition 7% were MRDneg and 16% MRDpos - both not fulfilling the criteria of MolCR or MolF (definitions see table). Results for OS at 5 yrs (MolCR vs MolF vs MRDneg vs MRDpos) were 83% vs 43% vs 78% vs 68% resp. and for RD 80% vs 38% vs 76% vs 56% resp. Differences were significant (p<.0001) for comparison of all groups, for MolCR vs MRDpos and MolCR vs MolF, but not for MolCR vs MRDneg.
In 196 MolF pts OS and RD from wk16 onward was 43% and 38% at 5 yrs resp. 121 (62%) MolF pts received SCT in ongoing 1st CR. The SCT rate in MolF pts increased from 54% (2003-2009) to 72% (2010-2016)(p=.008). OS and RD for non-SCT vs SCT pts was 28% vs 53% (p<.0001) and 9% vs 56% (p<.0001) at 5 yrs resp.
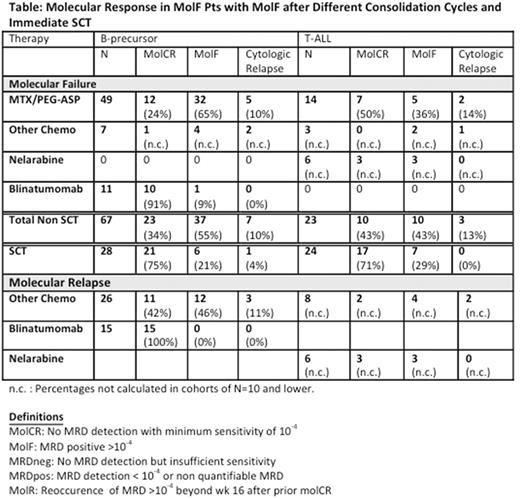
Out of 196 MolF pts, 19 relapsed shortly after wk 16, 2 pts were withdrawn, 1 pt died in CR and data were missing in 6 pts. Of the remaining 168 pts, 52 received immediate SCT (31%), whereas 115 pts received consolidation. Data on molecular response after the next 1-3 cycles or after SCT were available for 142 pts. In B-prec ALL (N=95) and T-ALL (N=47) the MolCR rate was 34% and 43% resp. for non-SCT approaches, whereas 75% and 71% resp. achieved a Mol CR after immediate SCT (table). However, the OS with immediate SCT vs later SCT was 34% (N=52) vs 63% (N=69) at 5 yrs resp (p=.002) and the corresp. RD was 42% vs 66% (p=.001) resp. Furthermore, pts with next consolidation leading to molCR had a superior OS (76% at 5yrs) vs those who did not (44% at 5yrs) (p=.02). A similar difference was seen for RD (60% vs 36% resp.; p=.08).
In addition 102 pts with MolR during/after chemo were observed (median time to MolR: 18 mo). OS and RD from MolR onwards were 51% and 35% at 5 yrs. 38 pts were transplanted in ongoing 1st CR. OS w/o and with SCT was 37% vs 71% (p=.001) resp. with corresp. RD of 5% vs 70% (p<.0001). Results of salvage therapies in 41 pts were comparable to those in MolF (table).
Important conclusions for future MRD based therapy can be drawn from this large adult ALL cohort: 1) a similar poor prognostic impact of MolF and MolR is underlined; 2) it is demonstrated that pts with any detectable MRD (MRDpos) have an intermediate prognosis and require regular follow-up MRD testing; 3) SCT offers an advantage in MolF and MolR pts, however 4) evidence was provided that later SCT (i.e. in better molecular status) could be superior to immediate SCT; 5) compliance with MRD testing and SCT in MolF increased over time; 6) many MolF pts relapsed quickly; 7) additional chemotherapy offered limited chances to achieve a MolCR, but 8) promising MolCR rates were observed for targeted therapies.
For future optimisation of MRD based therapy, logistics for decisions have been implemented earlier in the GMALL trial 08 in order to avoid rapid relapses. A first stratification takes place already after induction and targeted therapies are recommended in all MolF pts before SCT.
Rollig: Janssen: Research Funding; Bayer: Research Funding. Kneba: AbbVie: Consultancy, Honoraria, Other: travel support, Research Funding; F. Hoffmann-LaRoche: Consultancy, Honoraria, Other: travel support, Research Funding; Gilead: Consultancy, Honoraria, Other: travel support, Research Funding; Janssen-Cilag: Consultancy, Honoraria, Other: travel support, Research Funding; Mundipharma: Consultancy, Honoraria, Other: travel support, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal